Type 2 Diabetes Expert in Perumbakkam
Your Trusted Partner in Type 2 Diabetes
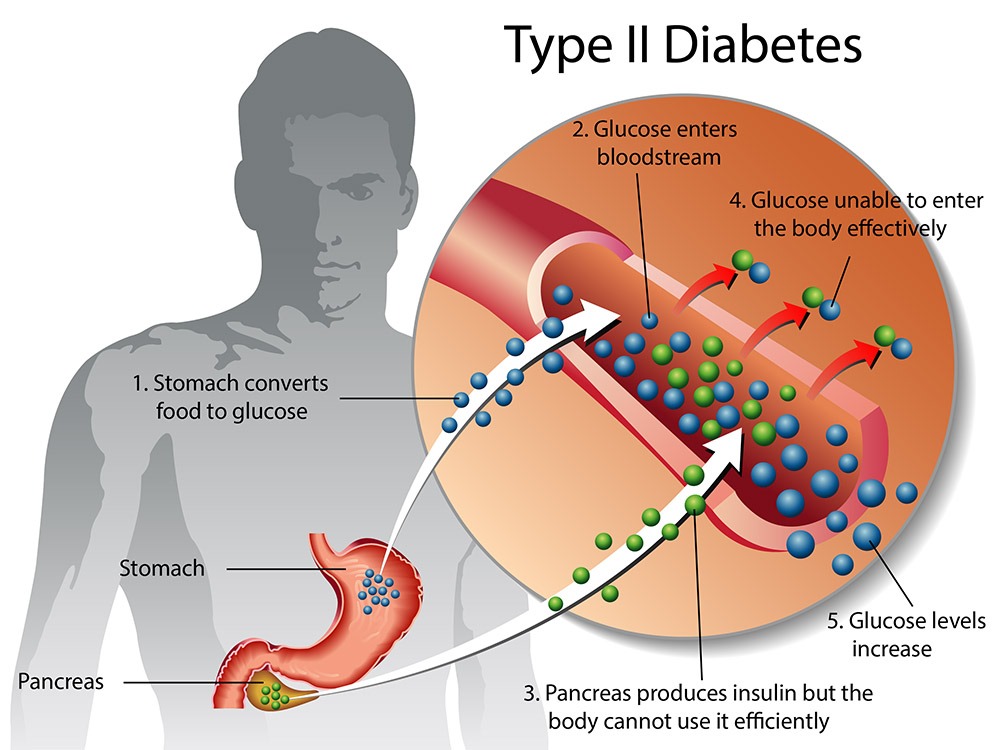
Type 2 diabetes is a chronic metabolic condition characterized by insulin resistance and relative insulin deficiency, leading to elevated blood sugar levels. Our dedicated team is committed to offering comprehensive care and support to individuals with Type 2 diabetes, providing personalized treatment plans and empowering them to effectively manage their condition for optimal health and well-being.

Understanding Type 2 Diabetes
Type 2 diabetes is a metabolic disorder characterized by insulin resistance, where the body’s cells become less responsive to insulin, and relative insulin deficiency, where the pancreas does not produce enough insulin to maintain normal blood sugar levels. This leads to hyperglycemia, or high blood sugar levels, which can cause long-term complications if left untreated. Unlike Type 1 diabetes, which is an autoimmune condition, Type 2 diabetes typically develops gradually over time and is often associated with lifestyle factors such as obesity, physical inactivity, and poor dietary choices.
The exact cause of Type 2 diabetes is multifactorial, involving a complex interplay of genetic, environmental, and lifestyle factors. Genetic predisposition plays a role, with certain genes increasing the risk of developing the condition. However, environmental factors such as sedentary lifestyle, unhealthy diet high in refined carbohydrates and sugars, and excess body weight are significant contributors to the development of insulin resistance and Type 2 diabetes. Aging also increases the risk of Type 2 diabetes, with the condition being more common in individuals aged 45 and older.
Managing Type 2 diabetes involves lifestyle modifications, including dietary changes, regular physical activity, and weight management, to improve insulin sensitivity and blood sugar control. Additionally, medication therapy may be necessary to lower blood sugar levels and reduce the risk of complications. Oral medications such as metformin, sulfonylureas, thiazolidinediones, DPP-4 inhibitors, SGLT2 inhibitors, and GLP-1 receptor agonists, as well as injectable insulin therapy, are commonly used to treat Type 2 diabetes and improve glycemic control.
Early detection and intervention are crucial for managing Type 2 diabetes and preventing complications. Regular monitoring of blood sugar levels, adherence to treatment regimens, and routine medical check-ups are essential for individuals with Type 2 diabetes to maintain optimal health and reduce the risk of cardiovascular diseases, neuropathy, nephropathy, retinopathy, and other diabetes-related complications. A multidisciplinary approach involving healthcare providers, dietitians, educators, and support networks can help individuals with Type 2 diabetes effectively manage their condition and improve their quality of life.
Causes of Type 2 Diabetes
Insulin Resistance: The primary cause of Type 2 diabetes is insulin resistance, where the body’s cells become less responsive to the effects of insulin. Insulin is a hormone that helps regulate blood sugar levels by facilitating the uptake of glucose from the bloodstream into cells for energy. When cells become resistant to insulin, glucose remains in the bloodstream, leading to high blood sugar levels.
Genetic Predisposition: Genetics plays a significant role in the development of Type 2 diabetes, with certain genetic factors increasing the risk of the condition. Individuals with a family history of Type 2 diabetes are at a higher risk of developing the condition themselves. However, genetic predisposition alone is not sufficient to cause Type 2 diabetes, and environmental factors also play a crucial role.
Lifestyle Factors: Unhealthy lifestyle choices, such as sedentary behavior, poor dietary habits, and excess body weight, are major contributors to the development of Type 2 diabetes. Lack of physical activity and a diet high in refined carbohydrates, sugars, and saturated fats can lead to weight gain, insulin resistance, and impaired glucose metabolism, increasing the risk of Type 2 diabetes.
Obesity: Excess body weight, particularly abdominal obesity or visceral fat, is strongly associated with an increased risk of Type 2 diabetes. Adipose tissue, especially visceral fat, releases pro-inflammatory cytokines and adipokines, which contribute to insulin resistance and inflammation. The accumulation of visceral fat around organs such as the liver and pancreas further impairs insulin sensitivity and glucose homeostasis.
Age: Age is a significant risk factor for Type 2 diabetes, with the prevalence of the condition increasing with advancing age. Aging is associated with changes in metabolism, decreased physical activity, loss of muscle mass, and increased adiposity, all of which contribute to insulin resistance and the development of Type 2 diabetes.
Ethnicity: Certain ethnic groups, including African Americans, Hispanic/Latino Americans, Native Americans, Asian Americans, and Pacific Islanders, have a higher prevalence of Type 2 diabetes compared to others. Genetic and environmental factors, as well as socioeconomic disparities, contribute to these ethnic disparities in diabetes risk.
Symptoms of Type 2 Diabetes:
- Frequent Urination (Polyuria)
- Increased Thirst (Polydipsia)
- Excessive Hunger (Polyphagia)
- Unexplained Weight Loss
- Fatigue and Weakness
- Blurred Vision
- Slow Healing of Wounds
- Tingling or Numbness in Hands or Feet
- Recurrent Infections
- Darkened Skin Patches
Treatments
Lifestyle Modifications:
- Healthy Eating: Adopting a balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can help regulate blood sugar levels and manage weight.
- Regular Physical Activity: Engaging in regular exercise, such as brisk walking, cycling, or swimming, for at least 150 minutes per week can improve insulin sensitivity and lower blood sugar levels.
- Weight Management: Achieving and maintaining a healthy weight through a combination of dietary changes and regular physical activity can reduce insulin resistance and improve glycemic control.
Medications:
- Oral Medications: There are several classes of oral medications used to treat Type 2 diabetes, including:
- Metformin: Improves insulin sensitivity and lowers blood sugar levels by decreasing glucose production in the liver and increasing glucose uptake by cells.
- Sulfonylureas: Stimulate insulin secretion from the pancreas to lower blood sugar levels.
- DPP-4 Inhibitors: Increase insulin secretion and decrease glucagon production to lower blood sugar levels.
- SGLT2 Inhibitors: Lower blood sugar levels by increasing glucose excretion in the urine.
- GLP-1 Receptor Agonists: Stimulate insulin secretion, suppress glucagon secretion, and slow gastric emptying to lower blood sugar levels.
- Injectable Medications: Injectable medications such as insulin or GLP-1 receptor agonists may be prescribed for individuals who cannot achieve glycemic control with oral medications alone.
Non-Surgical Treatments:
- Continuous Glucose Monitoring (CGM): CGM systems provide real-time glucose readings and trends, allowing individuals to monitor their blood sugar levels more closely and make adjustments to their treatment regimen as needed.
- Insulin Therapy: Insulin therapy may be initiated for individuals with Type 2 diabetes who cannot achieve glycemic control with oral medications alone. Insulin may be administered via injections or insulin pump therapy.
Surgical Intervention:
- Bariatric Surgery: Bariatric surgery may be considered for individuals with severe obesity and Type 2 diabetes who have not achieved adequate glycemic control with lifestyle modifications and medications. Bariatric surgery can lead to significant weight loss and improvement in insulin sensitivity, resulting in remission or improvement of Type 2 diabetes in some cases.
Frequently Asked Questions on Type 2 Diabetes
While Type 2 diabetes cannot always be prevented, lifestyle modifications such as maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet can significantly reduce the risk of developing the condition, especially in individuals with prediabetes.
Type 2 diabetes is diagnosed through blood tests to measure fasting blood glucose, oral glucose tolerance test (OGTT), or glycated hemoglobin (HbA1c) levels. Individuals with symptoms of diabetes or risk factors such as obesity or family history may undergo screening tests for early detection.
Untreated or poorly managed Type 2 diabetes can lead to serious complications, including cardiovascular diseases (heart attack, stroke), neuropathy (nerve damage), nephropathy (kidney damage), retinopathy (eye damage), foot problems (ulcers, infections), and other diabetes-related complications.
While there is no cure for Type 2 diabetes, it can often be managed effectively with lifestyle modifications and medication therapy. Some individuals may achieve remission of Type 2 diabetes with significant weight loss and lifestyle changes, but ongoing monitoring and management are typically necessary.
Diet and exercise play crucial roles in managing Type 2 diabetes by improving insulin sensitivity, lowering blood sugar levels, and promoting weight loss. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, combined with regular physical activity, can help control blood sugar levels and reduce the risk of complications.
Individuals with Type 2 diabetes can find support and resources through healthcare providers, diabetes education programs, support groups, online communities, and advocacy organizations.
