Coronary Artery Expert in Perumbakkam
Your Trusted Partner in Coronary Artery Disease
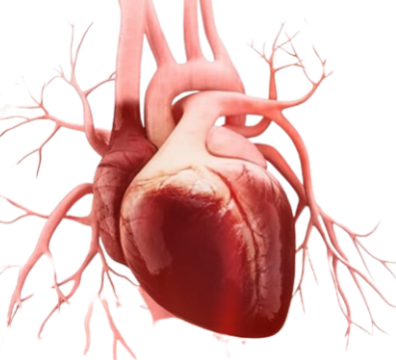
Coronary Artery Disease (CAD) is a cardiovascular condition where the blood vessels supplying the heart (coronary arteries) become narrowed or blocked, reducing blood flow.We are here to provide you with top-notch care and guidance to tackle your problems.

Understanding Coronary Artery Disease
Causes of Coronary Artery Disease
Coronary Artery Disease (CAD) is primarily caused by the buildup of plaque in the coronary arteries, a process known as atherosclerosis. This plaque consists of cholesterol, fat, and other substances, narrowing the arteries and restricting blood flow to the heart. Risk factors include high cholesterol, high blood pressure, smoking, diabetes, and a sedentary lifestyle.
Symptoms of Coronary Artery Disease:
- Anxiety or nervousness
- Shortness of Breath: Especially during physical activity
- Fatigue: Unusual tiredness
- Heart Attack
- Sudden chest pain
- pain radiating to the arm
- sweating
- Difficulty breathing
Risk factors
Coronary artery disease is common. Age, genetics, other health conditions and lifestyle choices can affect the health of the heart arteries.
Coronary artery disease risk factors include:
- Age: Getting older increases the risk of damaged and narrowed arteries.
- Sex: Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
- Family history: A family history of heart disease makes you more likely to get coronary artery disease. This is especially true if a close relative (parent, sibling) developed heart disease at an early age. The risk is highest if your father or a brother had heart disease before age 55 or if your mother or a sister developed it before age 65.
- Smoking: If you smoke, quit. Smoking is bad for heart health. People who smoke have a significantly increased risk of heart disease. Breathing in secondhand smoke also increases the risk.
- High blood pressure: Uncontrolled high blood pressure can make arteries hard and stiff (arterial stiffness). The coronary arteries may become narrow, slowing blood flow.
- High cholesterol: Too much bad cholesterol in the blood can increase the risk of atherosclerosis. Bad cholesterol is called low-density lipoprotein (LDL) cholesterol. Not enough good cholesterol — called high-density lipoprotein (HDL) — also leads to atherosclerosis.
- Diabetes: Diabetes increases the risk of coronary artery disease. Type 2 diabetes and coronary artery disease share some risk factors, such as obesity and high blood pressure.
- Overweight or obesity: Excess body weight is bad for overall health. Obesity can lead to type 2 diabetes and high blood pressure. Ask your health care provider what a healthy weight is for you.
- Chronic kidney disease: Having long-term kidney disease increases the risk of coronary artery disease.
- Not getting enough exercise: Physical activity is important for good health. A lack of exercise (sedentary lifestyle) is linked to coronary artery disease and some of its risk factors.
- A lot of stress: Emotional stress may damage the arteries and worsen other risk factors for coronary artery disease.
- Unhealthy diet: Eating foods with a lot of saturated fat, trans fat, salt and sugar can increase the risk of coronary artery disease.
- Alcohol use: Heavy alcohol use can lead to heart muscle damage. It can also worsen other risk factors of coronary artery disease.
- Amount of sleep: Too little and too much sleep have both been linked to an increased risk of heart disease.
Complications
Coronary artery disease can lead to:
- Chest pain (angina): When the coronary arteries narrow, the heart may not get enough blood when it needs it most — like when exercising. This can cause chest pain (angina) or shortness of breath.
- Heart attack: A heart attack can happen if a cholesterol plaque breaks open and causes a blood clot to form. A clot can block blood flow. The lack of blood can damage the heart muscle. The amount of damage depends in part on how quickly you are treated.
- Heart failure: Narrowed arteries in the heart or high blood pressure can slowly make the heart weak or stiff so it’s harder to pump blood. Heart failure is when the heart doesn’t pump blood as it should.
- Irregular heart rhythms (arrhythmias): Not enough blood to the heart can alter normal heart signaling, causing irregular heartbeats.
Prevention
- Healthy Lifestyle: Adopt a balanced diet, engage in regular exercise, and maintain a healthy weight.
- Quit Smoking: Smoking is a major risk factor; quitting can significantly reduce the risk.
- Manage Blood Pressure: Regular monitoring and management of hypertension.
- Control Cholesterol: Keep cholesterol levels in a healthy range through diet and medications if necessary.
- Manage Diabetes: Keep blood sugar levels under control.
- Regular Check-ups: Routine medical check-ups for early detection and management.
Treatment
- Medications: Including antiplatelets, statins, and medications to control blood pressure.
- Lifestyle Changes: Adopting a heart-healthy diet, regular exercise, and stress management.
- Angioplasty and Stent Placement: To open narrowed arteries.
- Coronary Artery Bypass Grafting (CABG): Surgical procedure for severe blockages.
- Cardiac Rehabilitation: A structured program for recovery and lifestyle modification.
Frequently Asked Question on Coronary Artery Disease
CAD is primarily caused by the buildup of plaque in coronary arteries, atherosclerosis, often influenced by factors like high cholesterol, high blood pressure, smoking, and diabetes.
Alcohol use disorder ranges from moderate to severe, with even mild cases having the potential to escalate and cause serious problems. If your drinking pattern causes significant distress and disrupts your daily life, it is likely indicative of alcohol use disorder.
Treatment may include medications, lifestyle changes, angioplasty with stent placement, coronary artery bypass surgery (CABG), and cardiac rehabilitation.
In many cases, lifestyle changes such as a heart-healthy diet, regular exercise, and smoking cessation can significantly manage CAD, especially in the early stages.
Diagnosis involves a combination of medical history, physical examination, imaging tests (like angiography), and blood tests.
