Anal Fissures Expert in Perumbakkam
Your Trusted Partner in Anal Fissures
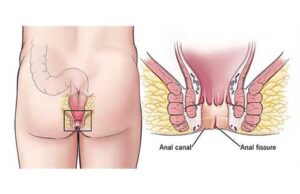
An anal fissure is a crack or split in the tissues that line your anal canal. Trauma causes the lining to tear, causing acute pain and bleeding. We are here to provide you with top-notch care and guidance to tackle your problems.

Understanding Anal Fissures
What is the main cause of an Anal Fissures?
Trauma — like stretching and straining — causes your anal lining to tear. But preexisting conditions can also play a role. This has to do with the antomy of your anal (butthole), which is really the last few centimeters of the long, muscular tube known as your large intestine.
Toward the end of your anus, where it opens to the outside, the skin is more like the skin on the outside of your body. But in the upper portion, where fissures usually happen, your anus is lined with the same soft mucosa as the rest of your large intestine.
This mucous lining is thinner and more delicate than normal skin, making it easier to tear. This is especially true for babies, who often get anal fissures. It can also become inflamed by injury or disease. Long-term (chronic) inflammation can weaken the tissues.
Your anus is surrounded by two circular muscles that help control your bowel movements (your anal sphincters). If these muscles are too tight, they can add tension to your anal lining, making it easier to tear and even reducing blood flow to the tissues.
Symptoms
- Sharp pain when pooping.
- Burning or itching with pooping.
- Fresh, red blood in your poop.
- Anal muscle spasms.
- A lump on the skin near the tear.
- List Item
Primary causes of Anal Fissures include:
- Chronic constipition and straining to poop.
- Obstructed defecation syndrome.
- Infant dyschezia
- Chronic diarrhea
- Childbirth.
- Penetration.
Other contributing conditions include:
- Prior surgery.
- Sexually transmitted infections(STIs)
- Inflammatory bowel diseases(IBD)
- Anal cancer
- Tuberculosis(TB)
- Diaper rash
What are the possible complications of Anal Fissures?
Many anal fissures heal by themselves in a few weeks, but complications can develop when they don’t. These are called chronic anal fissures. Instead of healing, they continue to reinforce themselves in a vicious cycle, leaving a persistent wound.
Pain and muscle clenching can cause your anal muscles to tighten and spasm. Muscle tension and anal spasms pull the fissure apart and reduce blood flow to the tissues. This makes it harder for it to heal, and also more painful, causing more tension.
If anal fissures go on too long without healing, they can lead to further complications, such as:
- Fecal impaction.
- Anal stenosis (narrowing of the anal canal that can make it harder to poop).
- Anal fistula.
How are Anal Fissures diagnosed?
A healthcare provider will ask you about your symptoms, then try to see the fissure. You’ll lie on your belly or on your side while they gently separate your buttocks. If this is too painful, they don’t have to go further. They can safely assume that you have an anal fissure.
But if you can tolerate an exam, they’ll try to see the fissure so that they can rule out other possible causes for your symptoms. They might gently insert a lubricated gloved finger to open your anus, noticing any tenderness or muscle spasms. This is a digital rectal exam.
What is the medical treatment for Anal Fissures?
When you have a chronic anal fissure — one that has lasted more than eight weeks — medical treatment focuses on relaxing the anal sphincter muscles that surround your anal canal. This should allow the fissure to begin to close and help restore blood flow to the tissues.
Medications
Medications for anal fissures include:
- Nitrolglycerin oitment: Nitroglycerin is a vasodilator, a medicine that makes your blood vessels expand. Applied as a cream, it can restore blood flow and can help your anal sphincter relax. However, it can cause headaches, and some people have to discontinue it for this reason.
- calcium channel blockers: such as diltiazem or nifedipine, are an alternative way of relaxing blood vessels and your anal muscles. These medications may work for you if nitroglycerin doesn’t.
- Botox: As a last resort, a Botox injection into your anal sphincter muscle can help relax it. Botox is a muscle relaxant. Its effects last for about three months, giving your fissure time to heal.
- Bulk Laxatives: Not everyone with constipation needs to take medication for it, but medications can help if you have very hard poops that cause additional stress on your anal fissure. Bulk laxatives, such as Metamucil (psyllium), draw fluid into your gut to help soften your poop.
How do you heal an Anal Fissures at home?
Most anal fissures will heal on their own, but you can help the process along with a little self-care. Here’s some advice:
- To make pooping more comfortable, consider a stool softner. Use a step stool to support your feet while sitting on the toilet, which helps position your hips in a squatting position.
- Wipe your anus carefully with soft paper or alcohol-free wet wipes. Consider using a bidet, or shower after pooping.
- Apply a topical ointment or cream to your fissure. Petroleum jelly can promote healing by sealing in moisture and acting as an antibiotic. Medicated creams can treat inflammation and pain.
- Take a sitz bath two or three times a day for at least 10-15 minutes. This is a shallow, warm water bath that you sit in to soak your anus. It can relieve your symptoms and help relax your muscles.
Should I adjust my diet while living with Anal Fissures?
It might help to:
- Drink more water.
- Eat more fresh fruits and vegetables.
- Avoid spicy foods and nuts while you have symptoms.
