Psoriasis IN PERUMBAKAM
Your Trusted Partner in Psoriasis
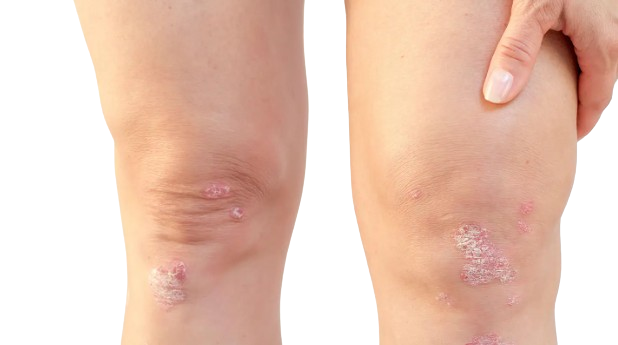
Psoriasis is a chronic autoimmune condition characterized by red, scaly patches on the skin. Despite being non-contagious, it can significantly impact one’s quality of life. At our clinic, we offer compassionate care and advanced treatments to manage your psoriasis effectively.
Understanding Psoriasis
What is Psoriasis?
Psoriasis is a chronic autoimmune condition that affects the skin, resulting in the rapid buildup of skin cells. This leads to the formation of thick, red patches covered with silvery scales, which can be itchy, painful, and sometimes even bleed. Psoriasis patches can appear anywhere on the body but are most commonly found on the elbows, knees, scalp, lower back, and nails. It is not contagious, but it can significantly impact a person’s physical and emotional well-being. Psoriasis is thought to be caused by a combination of genetic, immune system, and environmental factors, and it often runs in families. While there is no cure for psoriasis, various treatments can help manage symptoms and improve quality of life.
What are the types of Psoriasis?
Psoriasis manifests in several different forms, each presenting unique characteristics. The main types of psoriasis include:
Plaque Psoriasis:
- Plaque psoriasis is the most common form, characterized by raised, red patches covered with silvery-white scales. These patches often appear on the elbows, knees, scalp, and lower back.
Guttate Psoriasis:
- Guttate psoriasis typically appears as small, red, drop-like lesions on the skin. It often develops suddenly and is commonly triggered by bacterial infections, such as strep throat.
Inverse Psoriasis:
- Inverse psoriasis affects skin folds, such as the armpits, groin, and under the breasts. It appears as smooth, red patches of inflamed skin and may worsen with friction and sweating.
Pustular Psoriasis:
- Pustular psoriasis is characterized by pus-filled blisters surrounded by red skin. It can occur in localized areas or widespread across the body and may be accompanied by fever and chills.
Erythrodermic Psoriasis:
- Erythrodermic psoriasis is a severe and rare form of psoriasis that causes widespread redness and shedding of the skin. It can be life-threatening and requires immediate medical attention.
Nail Psoriasis:
- Nail psoriasis affects the nails, causing changes such as pitting, discoloration, thickening, and crumbling. It can be challenging to treat and may cause discomfort or functional impairment.
Scalp Psoriasis:
- Scalp psoriasis appears on the scalp as red, itchy, and scaly patches. It can extend beyond the hairline onto the forehead, neck, and behind the ears. It may also lead to temporary hair loss.
What are the symptoms of Psoriasis?
Red Patches: Raised, inflamed patches of skin, typically covered with silvery-white scales.
Itching or Burning Sensation: Pruritus or burning sensation in affected areas, leading to discomfort.
Thickened or Cracked Skin: Skin may become thickened, cracked, or develop fissures, especially on the palms, soles, or joints.
Silvery-White Scales: Scales of dead skin cells that may flake off or be shed, leaving behind a shiny or silver appearance.
Dry, Scaly Skin: Dryness and scaling of the skin, often accompanied by irritation and shedding.
Pitting or Discoloration of Nails: Changes in the nails, such as pitting, discoloration, thickening, or crumbling.
Joint Pain or Swelling: Psoriatic arthritis may cause joint pain, stiffness, and swelling, particularly in the fingers and toes.
Bleeding or Cracking: Skin may bleed or crack due to dryness, especially in areas prone to friction or movement.
Discomfort or Pain: Discomfort or pain associated with psoriatic lesions, especially if they are large or located in sensitive areas.
Emotional Impact: Psychological distress, including stress, depression, or anxiety, due to the visible nature of the condition and its impact on daily life.
What causes Psoriasis?
Genetic Factors: Psoriasis has a strong genetic component, with a family history of the condition increasing the likelihood of developing it.
Immune System Dysfunction: Psoriasis is considered an autoimmune disorder, where the immune system mistakenly attacks healthy skin cells, leading to inflammation and the rapid turnover of skin cells.
Environmental Triggers: Various environmental factors, such as stress, infections (particularly streptococcal infections), injuries to the skin (e.g., cuts, burns), and certain medications (e.g., lithium, beta-blockers), can trigger or exacerbate psoriasis flare-ups.
Hormonal Changes: Hormonal changes, such as those occurring during puberty, pregnancy, or menopause, may influence the onset or severity of psoriasis symptoms.
Obesity and Metabolic Syndrome: There is evidence to suggest that obesity and metabolic syndrome may increase the risk of developing psoriasis or exacerbate existing symptoms.
Smoking and Alcohol Consumption: Smoking and excessive alcohol consumption have been associated with an increased risk of psoriasis and may worsen symptoms in individuals already affected by the condition.
Psychological Factors: Stress, anxiety, and depression can contribute to psoriasis flare-ups or worsen existing symptoms through their impact on the immune system and inflammatory processes.
Dietary Factors: While the role of diet in psoriasis is not fully understood, some individuals may find that certain foods or dietary habits trigger or worsen their symptoms.
Skin Trauma or Irritation: Physical trauma to the skin, such as scratches, sunburns, or friction, can trigger the development of psoriasis lesions, known as the Koebner phenomenon.
Altered Skin Microbiome: Disruption of the balance of microorganisms on the skin, known as the skin microbiome, may play a role in the development or exacerbation of psoriasis.
How do you treat Psoriasis?
The treatment of psoriasis aims to reduce inflammation, alleviate symptoms, and improve the quality of life for individuals affected by the condition. Treatment approaches vary depending on the severity of symptoms, the type of psoriasis, and individual factors such as age and overall health. Topical treatments, such as corticosteroids, vitamin D analogs, and retinoids, are often used to manage mild to moderate psoriasis by reducing inflammation and controlling skin cell turnover. Phototherapy, or light therapy, involves exposing the skin to ultraviolet light, which can slow the growth of skin cells and reduce inflammation. For more severe cases or psoriasis resistant to other treatments, systemic medications such as oral retinoids, methotrexate, cyclosporine, or biologic drugs may be prescribed to target the underlying immune system dysfunction. Additionally, lifestyle modifications, including stress management, maintaining a healthy weight, avoiding triggers, and moisturizing the skin, can help manage psoriasis symptoms and improve overall well-being. It’s essential for individuals with psoriasis to work closely with healthcare providers to develop a comprehensive treatment plan tailored to their specific needs and goals.
Frequently Asked Question on Psoriasis
Psoriasis is associated with an increased risk of other health conditions, including cardiovascular disease, diabetes, obesity, depression, and anxiety. It’s essential for individuals with psoriasis to receive regular medical care and screenings for these conditions.
- Psoriasis is typically diagnosed based on a physical examination, medical history, and sometimes a skin biopsy to confirm the diagnosis.
Yes, psoriasis can also affect the nails, joints, and other parts of the body, leading to conditions such as psoriatic arthritis.
Psoriasis flare-ups can be triggered by factors such as stress, infections, injuries to the skin, certain medications, hormonal changes, smoking, alcohol consumption, and dietary factors.
No, psoriasis is not contagious. It is an autoimmune disorder caused by an overactive immune system, not by bacteria or viruses.
