Cataract Surgery Expert in Perumbakkam
Your Trusted Partner in Cataract Surgery
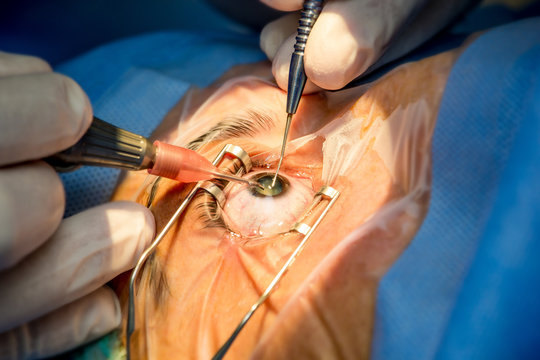
Healthcare providers use cataract surgery to remove clouded lenses in the eye, restoring clear vision and improving visual acuity. We are dedicated to offering comprehensive care and guidance throughout the cataract surgery process, ensuring optimal outcomes and improved vision for our patients.
Understanding Cataract Surgery
What is Cataract Surgery?
Cataract surgery is a common medical procedure performed to treat cataracts, which are cloudy areas that develop in the lens of the eye, leading to blurred vision and visual impairment. During the surgery, the cloudy lens is removed and replaced with an artificial intraocular lens (IOL) to restore clear vision. Cataract surgery is typically performed on an outpatient basis and is considered one of the safest and most effective surgical procedures, resulting in improved vision and quality of life for individuals affected by cataracts.
What are Cataract Surgery Types?
There are two main types of cataract surgeries:
Phacoemulsification (Phaco): Phacoemulsification, or phaco, is the most common type of cataract surgery performed today. It involves the use of ultrasound energy to break up the cloudy lens (cataract) into small pieces, which are then suctioned out through a small incision in the eye. Once the cataract is removed, an artificial intraocular lens (IOL) is inserted into the eye to replace the natural lens and restore clear vision. Phacoemulsification is a minimally invasive procedure that typically requires a small incision and often results in rapid visual recovery.
Extracapsular Cataract Extraction (ECCE): Extracapsular cataract extraction (ECCE) is an older technique that involves removing the cloudy lens in one piece through a larger incision in the eye. Unlike phacoemulsification, which breaks up the cataract into smaller fragments, ECCE requires a larger incision to remove the entire lens intact. After removal, an IOL is inserted into the eye to replace the natural lens. ECCE is less commonly performed today, as phacoemulsification has become the preferred method for cataract surgery due to its smaller incision size, faster recovery times, and reduced risk of complications. However, ECCE may still be used in certain cases, such as when phacoemulsification is not feasible or in combination with other surgical techniques.
What happens before this procedure?
Before cataract surgery, several steps are typically taken to ensure the procedure is safe and successful:
Comprehensive Eye Examination: The ophthalmologist will conduct a thorough eye examination to assess the extent of the cataract and determine if cataract surgery is necessary. This examination may include visual acuity tests, pupil dilation, and measurements of the eye’s shape and size.
Discussion of Treatment Options: The ophthalmologist will discuss treatment options with the patient, including the benefits and risks of cataract surgery, as well as alternative treatments such as eyeglasses or contact lenses.
Selection of Intraocular Lens (IOL): If cataract surgery is recommended, the patient will have the opportunity to choose the type of intraocular lens (IOL) to be implanted during the procedure. Different types of IOLs offer varying benefits, such as improved distance vision, near vision, or reduced dependence on glasses.
Preoperative Testing: Before surgery, the patient may undergo preoperative testing to assess overall health and identify any potential risk factors or medical conditions that could affect the surgery or anesthesia. This may include blood tests, electrocardiogram (ECG), and evaluation by other specialists if needed.
Medication Review: The patient will be instructed on which medications to continue or discontinue before surgery, particularly blood thinners or medications that may affect anesthesia or postoperative healing.
Instructions for Surgery Day: The patient will receive instructions for the day of surgery, including when to stop eating and drinking before the procedure, what medications to take, and what to expect during and after surgery. It’s essential to follow these instructions closely to ensure a smooth and successful surgical experience.
What happens during these Surgeries?
During cataract surgery, whether it’s phacoemulsification or extracapsular cataract extraction (ECCE), the basic steps involve the following:
Anesthesia: Before the surgery begins, the eye is numbed using local anesthesia, typically administered via eye drops or injections around the eye. In some cases, sedation may also be given to help the patient relax.
Incision: A small incision is made in the cornea or sclera (the white part of the eye) to access the cataract. The size and location of the incision may vary depending on the type of surgery and the surgeon’s preference.
Lens Removal: In phacoemulsification, ultrasound energy is used to break up the cloudy lens (cataract) into small fragments, which are then suctioned out of the eye through the incision. In ECCE, the cataract is removed intact through a larger incision.
IOL Implantation: After the cataract is removed, an artificial intraocular lens (IOL) is implanted into the eye to replace the natural lens. The IOL is typically folded or rolled up and inserted through the same incision used for lens removal. Once inside the eye, the IOL unfolds or expands to its proper position.
Closure: The incision is carefully closed using self-sealing techniques or sutures, depending on the type of surgery and the surgeon’s preference. Sutures may be used in ECCE or in certain cases where additional wound support is needed.
Postoperative Care: After the surgery is complete, the patient is monitored for a short period in the recovery area. Eye drops or ointments may be prescribed to prevent infection and promote healing. The patient is usually able to go home the same day, although someone else may need to drive them.
What happens after Cataract Surgery?
If you received general anesthesia, you’ll rest in a recovery room while your anesthesia wears off. If you had local anesthesia, you’lAfter cataract surgery, patients typically experience improved vision, although some temporary side effects may occur. It’s essential to follow postoperative instructions provided by the surgeon, including using prescribed eye drops, avoiding strenuous activities, and attending follow-up appointments. Most patients can resume normal activities within a few days, but full recovery may take several weeks. It’s important to report any persistent pain, redness, or vision changes to the surgeon promptly. With proper care, cataract surgery usually leads to significant vision improvement and enhanced quality of life.l be able to go home right away. Before you leave, your provider will give you information about taking care of yourself as you recover. Your provider may prescribe pain medication to help with the mild or moderate pain you may have for a week or so after your surgery. They may also prescribe antibiotics to help prevent infection.
What are the risks or complications of Cataract Surgery?
While cataract surgery is generally considered safe and effective, like any surgical procedure, it carries certain risks and potential complications. Some of these risks include:
Infection: There is a small risk of developing an eye infection after cataract surgery, which may require antibiotic treatment.
Inflammation: Inflammation inside the eye (called uveitis) can occur after surgery and may require anti-inflammatory medication to control.
Swelling: Swelling of the cornea or retina may occur, affecting vision temporarily. This usually resolves with time or may require additional treatment.
Increased Intraocular Pressure (IOP): Some patients may experience a temporary increase in intraocular pressure (IOP) after surgery, which can be managed with medication or further intervention.
Posterior Capsule Opacification (PCO): In some cases, the capsule behind the IOL may become cloudy over time, leading to blurred vision. This can be treated with a laser procedure called YAG laser capsulotomy.
Retinal Detachment: While rare, retinal detachment can occur after cataract surgery. Symptoms include sudden flashes of light, floaters, or a curtain-like shadow over the vision. Prompt medical attention is necessary if these symptoms occur.
Corneal Edema: Swelling of the cornea can occur after surgery, leading to temporary vision disturbances. This usually resolves with time or may require treatment with eye drops.
IOL Dislocation or Decentration: The intraocular lens (IOL) implanted during surgery may shift position or become dislocated, affecting vision. This may require additional surgery to reposition or replace the IOL.
Glaucoma: Cataract surgery may increase the risk of developing glaucoma or exacerbate preexisting glaucoma in some patients. Close monitoring of intraocular pressure is essential.
Visual Symptoms: Some patients may experience glare, halos, or difficulty with night vision after cataract surgery, particularly in the early postoperative period. These symptoms usually improve over time as the eye heals.
Is Cataract Surgery worth it?
Yes, cataract surgery is often considered highly worthwhile for individuals experiencing vision impairment due to cataracts. The procedure is safe, effective, and minimally invasive, with a high success rate in restoring clear vision and improving quality of life. Most patients experience significant vision improvement soon after surgery, allowing them to resume daily activities with greater independence and confidence.
How long does it take to recover from Cataract Surgery?
Recovery from cataract surgery is typically relatively quick, with most patients experiencing improved vision within a few days to weeks after the procedure. While individual recovery times may vary, many people are able to resume normal activities, such as driving and work, within a few days after surgery. However, it’s essential to follow postoperative instructions provided by the surgeon, including using prescribed eye drops, avoiding strenuous activities, and attending follow-up appointments. Full recovery, including stabilization of vision and healing of the eye, may take several weeks. It’s important to report any persistent pain, redness, or vision changes to the surgeon promptly during the recovery period.
Frequently Asked Question on Cataract Surgery
Cataract surgery is a procedure to remove the cloudy lens (cataract) from the eye and replace it with an artificial intraocular lens (IOL) to restore clear vision.
You may need cataract surgery if cataracts are causing significant vision impairment that affects your daily activities, such as driving, reading, or watching TV.
Yes, cataract surgery is considered safe and is one of the most commonly performed surgical procedures worldwide.
Cataract surgery typically takes less than an hour to perform, although the exact duration may vary depending on the complexity of the case.
No, cataract surgery is usually painless. Local anesthesia is used to numb the eye, and you may receive sedation to help you relax during the procedure.
Most patients experience improved vision within a few days to weeks after cataract surgery. Full recovery may take several weeks.
The results of cataract surgery are typically long-lasting, with most patients experiencing improved vision for many years after the procedure. However, the artificial IOL may need to be replaced or adjusted in rare cases.
